Suboxone is a medication used to treat opioid addiction and is an essential tool to battle against the opioid epidemic in the United States. It contains two key ingredients: buprenorphine and naloxone. It works by interacting with receptors in the brain.
When used as directed under medical supervision, Suboxone helps individuals overcome substance use disorder while minimizing the potential for abuse and dependence on this drug. It’s important to check in regularly with your doctor and take the medicine exactly as they tell you. That helps make sure the treatment works well and reduces any unwanted effects.
Key Takeaways
Suboxone combines buprenorphine and naloxone, addressing opioid challenges and fostering recovery. Here’s what you need to know:
- Suboxone curbs cravings by mimicking opioid effects, aiding recovery without intense highs.
- Adherence to prescribed schedules and regular healthcare consultations optimize Suboxone’s safety and effectiveness.
- Suboxone, alongside counseling, provides a holistic approach to sustained recovery from opioid addiction.
The Haven Detox-Little Rock is here to help you overcome opioid addiction. Contact us today at (501) 271-3342.
Understanding Suboxone
Suboxone, a key tool in treating opioid addiction, is a medication designed to help people break free from the challenges of substance dependence. This drug contains key components, buprenorphine and naloxone. Let’s delve into the specifics of how Suboxone, with its unique composition, addresses opioid-related challenges and facilitates the path to recovery.
Buprenorphine and Naloxone
Within Suboxone, buprenorphine acts as a partial opioid agonist, interacting with opioid receptors in the brain in the same way as other opiates.
The effects of this are somewhat weaker than those of other substances, such as heroin or prescription painkillers. By attaching itself to opioid receptors, buprenorphine works to reduce cravings for more potent substances. Naloxone, an opioid antagonist, is included to deter misuse, creating a balance that aids patients on their journey to sobriety.
How Suboxone is Administered
Individuals place Suboxone under their tongue. That is called a “sublingual” method, and it helps the medicine get absorbed best. The usual starting dose involves placing one or two films or tablets under the tongue. That can be adjusted as needed during treatment.
Suboxone Interaction With Brain Chemicals
It’s crucial to grasp how opioids affect the brain before understanding how Suboxone works. This will help you to see how Suboxone interacts with the neural pathways to address opioid dependence.
When opioids are consumed, they bind to opioid receptors in the brain. Chronic opioid use can lead to the development of tolerance, where higher doses are needed to achieve the same level of pain relief or euphoria.
Buprenorphine binds to the same opioid receptors in the brain that other opioids bind to. Since it is a partial agonist, it activates these receptors to a lesser extent compared to full agonists such as morphine.
Buprenorphine, a partial opioid agonist, mimics opioids’ effects without producing the same intensity, while naloxone prevents misuse by blocking opioid receptors. This dual action promotes a controlled balance, aiding individuals during recovery at the rehab center.
Effects of Suboxone on Opiate Addiction
Suboxone emerges as an effective treatment in combating opiate dependence, particularly in the context of heroin or opioid misuse. Here is how it is used in different levels of care:
Suboxone in Detox
In detox, Suboxone stands out as a crucial player. Its inclusion as part of medication-assisted treatment (MAT) offers a controlled transition, mitigating the harsh withdrawal effects such as vomiting and body aches that occur due to the absence of opioids in the body.
MAT treatment is often started after a person has abstained from using opioids for a certain period, typically when they are already in the early stages of withdrawal. This measured approach, often involving doctors, underscores the significance of Suboxone in fostering a safer and more manageable detoxification process.
Suboxone and Cravings
Cravings pose a significant challenge in opioid dependence, and Suboxone addresses this by reducing the desire for short-acting opioids. Its combination of buprenorphine and naloxone provides a balanced effect, curbing cravings without producing the same intense high effect as full agonist drugs.
Safe Path to Use Suboxone
Safe Suboxone use requires suitable prescription dosage and following the doctor’s directions. Misusing this drug can lead to dependence and addiction.
The safe use of Suboxone is paramount in its role as an FDA-approved medication for opioid addiction. Healthcare professionals play a crucial role in guiding patients through its proper utilization. Ensuring an appropriate dose of buprenorphine, typically administered through sublingual tablets, is key.
Patients are advised to adhere strictly to prescribed schedules, recognizing the significance of not missing doses. Regular consultations with healthcare professionals help fine-tune the treatment plan, optimizing its effectiveness.
Risk of Misuse
Despite its benefits, the misuse of Suboxone poses risks that necessitate caution. Deviating from prescribed doses increases the risk of overdose, highlighting the importance of strict adherence to healthcare professionals’ guidance.
Suboxone is beneficial for addiction recovery, but it’s not a standalone solution. It works best when used along with counseling and support.
Always talk to your healthcare team if you have any questions or concerns. Open communication with healthcare professionals about any concerns or adverse reactions provides a safer and more effective integration of Suboxone into the recovery journey.
Adverse Effects of Suboxone You Should Know
Suboxone, a cornerstone in opioid addiction treatment, brings relief to individuals seeking recovery. However, it’s essential to grasp potential side effects to make informed choices and manage well-being effectively.
Common Side Effects
During the initial stages of Suboxone treatment, individuals may experience mild and temporary side effects. Nausea, a common occurrence, can often be reduced by taking Suboxone with food. Headaches and constipation are also reported but are typically manageable and tend to diminish over time.
Severe Side Effects
While rare, Suboxone may lead to severe side effects, including respiratory depression. This condition involves dangerously slowed breathing and necessitates immediate medical attention. Individuals should promptly report any difficulty breathing or chest pain to their healthcare providers. Moreover, an allergic reaction to any of the ingredients in Suboxone is rare but may cause itching and dizziness if it happens.
Watching out for these severe side effects highlights why it’s essential to talk to the doctor regularly. Regular check-ins with medical professionals ensure the Suboxone treatment is safe and working well. It’s a way to ensure that the experience with Suboxone is secure and effective in helping with the recovery journey.
Withdrawal Effects
Withdrawal from Suboxone (buprenorphine/naloxone) can occur when the medication is abruptly discontinued after prolonged use.
Common withdrawal symptoms include:
- Nausea
- Vomiting
- Muscle aches
- Joint pain
- Runny nose
Some of the psychological symptoms include:
- Anxiety
- Restlessness
- Irritability
The severity and duration of withdrawal symptoms vary among individuals, depending on factors like dosage, duration of use, and individual differences. To minimize discomfort, doctors use the taper-off method under medical supervision.
Suboxone as a Long-Term Treatment Option
Suboxone’s role as a long-term treatment option is significant in supporting individuals on the path to sustained opioid addiction recovery. Delving into its impact on both physical and mental health, as well as comparing it to alternative opioid addiction treatment options, provides valuable insights for those considering extended use.
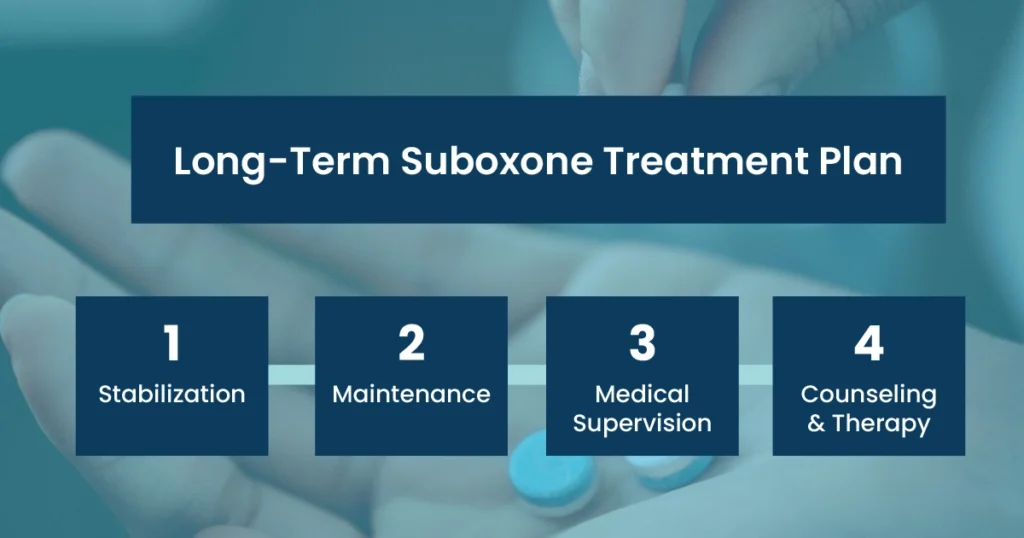
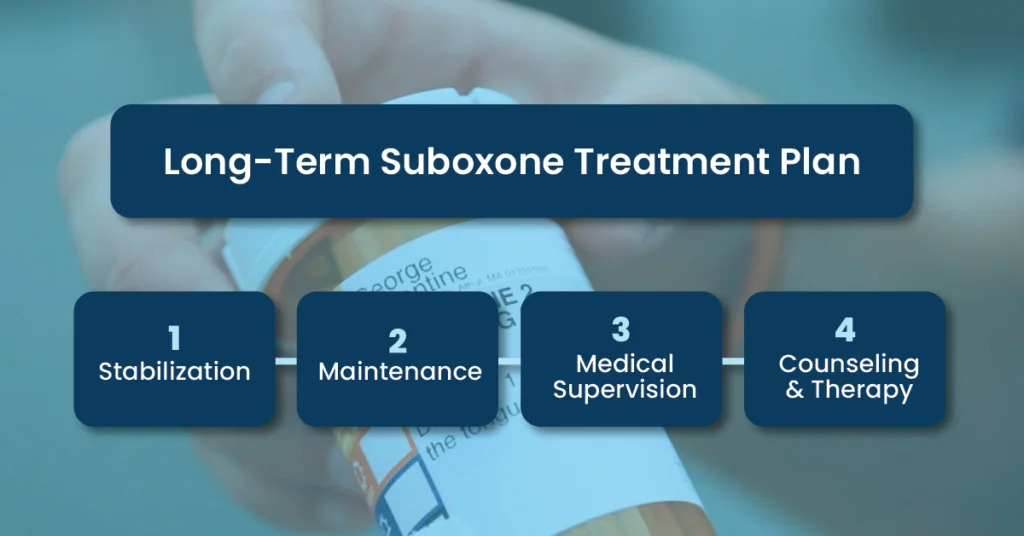
Stabilization
In the initial phase of treatment, individuals are typically stabilized on an appropriate dose of Suboxone. That helps alleviate withdrawal symptoms and cravings associated with opioid dependence.
Maintenance
Once stabilized, the individual may continue on a maintenance dose for an extended period. Factors like the severity of addiction, how a person responds to treatment, and if they have mental health issues can influence how long maintenance treatment lasts.
Medical Supervision
Long-term Suboxone treatment is given under medical supervision. Regular visits to a healthcare provider are essential to monitor progress, adjust medication dosage if necessary, and address any concerns or side effects.
Counseling and Behavioral Therapy
Medication-assisted treatment with Suboxone is often most effective when combined with counseling and behavioral therapy. This comprehensive approach helps address the underlying issues contributing to opioid dependence and promotes long-term recovery.
Frequently Asked Questions (FAQ)
Starting Suboxone initiates relief from opioid cravings and withdrawal symptoms. Typically taken under the tongue, an individual can experience its effects within hours.
It’s vital to adhere to your doctor’s plan for optimal results. While some may encounter mild side effects like nausea initially, these often diminish over time as your body adjusts to the medication. Continuous communication with healthcare professionals ensures a tailored and practical Suboxone experience.
Indeed, Suboxone exhibits positive impacts on mental health. By managing opioid dependence, it commonly alleviates anxiety and enhances mood. However, individual responses may vary, emphasizing the importance of communicating any mental health concerns or changes with your healthcare team for personalized guidance and support.
Long-term use of Suboxone contributes to stable physical and mental health. Effectively managing cravings and reducing anxiety, it fosters an environment conducive to overall well-being.
Regular check-ins with healthcare providers are crucial in ensuring a balanced and sustained approach to recovery. Even though everyone’s experience is different, talking a lot with your healthcare team is essential. That helps them monitor how Suboxone works for you in the long run.
Find Hope to Recovery at The Haven Detox-Little Rock
If you or a loved one is grappling with the challenging journey of opioid use disorder, The Haven Detox-Little Rock is here to offer a helping hand. We understand the struggle, and our dedicated team is committed to providing opioid addiction treatment and support.
Our comprehensive services include detox, ensuring a safe and comfortable transition from opioid dependence. Our residential rehab program offers a structured and nurturing environment for lasting recovery.It is time to take the first step toward a brighter future. Contact us at (501) 271-3342. Your path to recovery begins here.




