Medications play an important role in alleviating the challenging symptoms associated with discontinuing opioid use.
From agonists that mimic opioid effects to antagonists that block their action, these medications offer diverse approaches.
Let’s explore medications for opioid withdrawal, shedding light on their mechanisms, benefits, and the hope they bring to those seeking to break free from the grip of addiction.
Key Takeaways
Individualized treatment plans, with proper dosage management and monitoring, optimize medication benefits in opioid withdrawal. Here’s what you need to know:
- Buprenorphine-naloxone combination therapy reduces cravings and opioid withdrawals.
- Clonidine, an alpha-2 adrenergic agonist, eases withdrawal discomfort by targeting autonomic symptoms during opioid detox.
- Combining medication with behavioral therapies can help in addressing the physical and psychological aspects of addiction.
Contact The Haven Detox-Little Rock at (501) 271-3342 for more information.
Opioid Withdrawal Explained
Opioids, a class of drugs primarily prescribed for chronic pain management, include opioid analgesics and synthetic drugs. These potent substances bind to specific receptors in the brain, diminishing pain signals.
When individuals abruptly cease opioid intake, they often experience withdrawal symptoms. This challenging phase involves physical and psychological distress, such as nausea, anxiety, and muscle aches.
Opioid Withdrawal Timeline
Opioid withdrawal is a challenging process that occurs when individuals who have been using synthetic opioids suddenly stop or significantly reduce their intake. The timeline of opioid withdrawal can vary from person to person based on factors such as the type and amount of opioid used, the duration of use, and individual differences in metabolism.
Withdrawal symptoms typically follow a general timeline, which can be broken down into several stages.
Early Withdrawal (6-12 hours)
The early stage of opioid withdrawal usually begins within 6 to 12 hours after the last opioid use. During this phase, individuals may experience initial symptoms such as muscle aches, insomnia, anxiety, agitation, and infectious diseases.
These early signs often accompany flu-like symptoms, including yawning, runny nose, and excessive tearing. The onset of these symptoms is a clear indication that the body is reacting to the absence of opioids.
Peak Withdrawal (1-3 days)
The peak of opioid withdrawal typically occurs between 24 and 72 hours after the last opioid use. Intensified symptoms, including severe cravings, nausea, vomiting, diarrhea, abdominal cramps, and sweating characterize this stage.
Individuals may also experience dilated pupils, elevated heart rate, and increased blood pressure. The physical and psychological distress during this period can be particularly challenging, and the risk of relapse is often high.
Subacute Withdrawal (4-7 days)
After the initial peak, withdrawal symptoms gradually begin to subside during the subacute phase, which usually spans from the fourth to the seventh day. While some physical symptoms may persist, the intensity generally diminishes.
However, psychological symptoms such as anxiety, irritability, and mood swings may still be prominent. Sleep disturbances can continue to be an issue during this stage.
Post-Acute Withdrawal (Weeks to Months)
For some individuals, a prolonged phase known as post-acute withdrawal syndrome (PAWS) may occur, lasting for weeks to months. Although the acute physical symptoms have largely subsided, individuals may still experience lingering psychological symptoms.
Common PAWS symptoms include anxiety, depression, fatigue, and difficulty concentrating. Cravings for opioids may persist, and individuals may find it challenging to engage in daily activities fully.
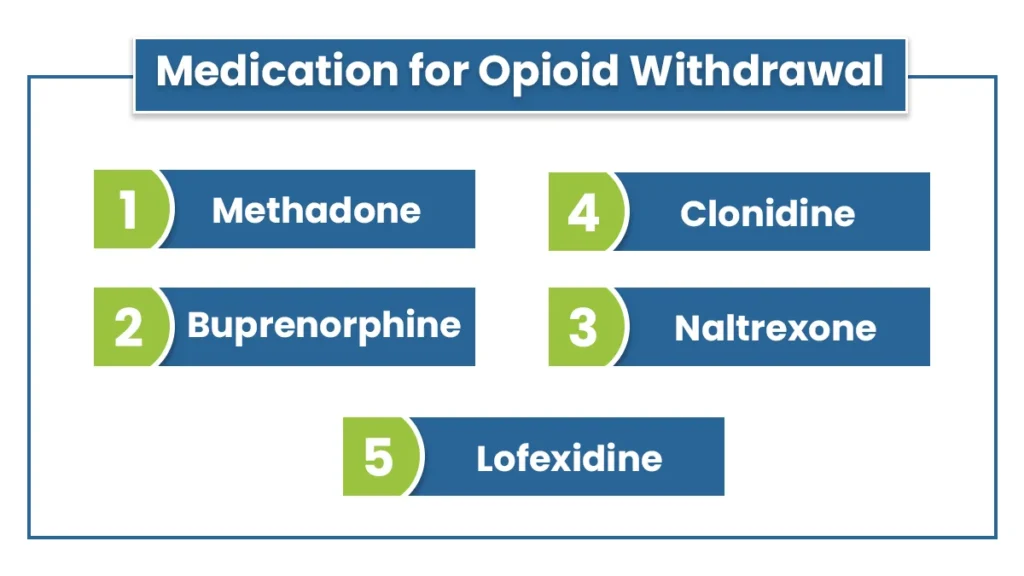
Medication for Opioid Withdrawal
Medications are often used to alleviate opioid withdrawal symptoms and facilitate a smoother recovery process. Several medications have proven effective in managing withdrawal symptoms.
Methadone
Methadone is a long-acting opioid agonist that helps reduce cravings and withdrawal symptoms. It works by binding to the same receptors in the brain that opioids target, providing a similar but less intense effect.
Methadone is often administered through a supervised clinic, allowing for close monitoring and adjustment of dosage. This medication has been a mainstay in opioid addiction treatment for decades, helping individuals stabilize their lives and reduce the risk of relapse.
Buprenorphine
Buprenorphine is a partial opioid agonist that binds to the same receptors as opioids but produces weaker effects. It helps reduce cravings and withdrawal symptoms without causing the same euphoria as other opioids. Buprenorphine is often combined with naloxone to deter misuse.
This medication can be prescribed by qualified healthcare providers, offering a more accessible option for some individuals compared to methadone.
Naltrexone
Naltrexone is an opioid antagonist that blocks opioid receptors, preventing the euphoric effects of opioids. Unlike methadone and buprenorphine, naltrexone is non-addictive. It can be administered orally or through a monthly injection, providing flexibility for individuals in recovery.
Naltrexone is particularly useful for those motivated to abstain from opioid drugs, as its effectiveness relies on compliance with the treatment plan.
Clonidine
Clonidine is a non-opioid medication that helps manage certain withdrawal symptoms, such as anxiety, agitation, and high blood pressure. While it does not directly address opioid cravings, clonidine can improve overall comfort during the withdrawal process.
It is often used as an adjunct medication in combination with other treatments.
Lofexidine
Lofexidine is another non-opioid medication used to alleviate withdrawal symptoms, specifically targeting the sympathetic nervous system. It helps reduce sweating, muscle aches, and runny nose.
Lofexidine is approved for use in the United States to manage withdrawal and can be a valuable component of a comprehensive treatment plan for opioid use disorder.
Precautions in Medically-Assisted Detox
Medically-assisted detoxification is a process in which individuals undergo withdrawal from illegal substances such as drugs or alcohol under the supervision of medical professionals. This process involves the use of medications to manage withdrawal symptoms and complications.
It’s crucial to take certain precautions during medically assisted detox to ensure the safety and well-being of the individual undergoing the process.
Here are some key precautions:
- Medical Assessment: Before starting opioid detox, a comprehensive medical assessment should be conducted to evaluate the individual’s overall health, medical history, and pre-existing conditions.
- Professional Supervision: Detox should be conducted under the supervision of qualified medical providers, such as doctors, physicians, nurses, and addiction specialists.
- Individualized Treatment Plans: Each person’s detoxification needs are unique. Individualized treatment plans should be developed based on the specific substance use, health status, and other relevant factors.
- Withdrawal Symptom Management: Medications should be used to manage withdrawal symptoms, including slow heart rate, low blood pressure, and respiratory depression effectively.
- Psychological Support: Emotional and psychological support is crucial during detox. Counseling, therapy, and support groups can help patients cope with the psychological aspects of Withdrawal.
- Hydration and Nutrition: Adequate hydration and nutrition are important for the individual’s overall well-being. Dehydration and malnutrition can exacerbate withdrawal symptoms and prolong the detoxification process.
- Gradual Tapering: In some cases, a gradual tapering of the substance may be recommended instead of abrupt cessation to minimize withdrawal symptoms.
- Emergency Preparedness: treatment facilities providing medically assisted detox should be equipped to handle medical emergencies. Emergency medical protocols should be in place, and staff should be trained to respond promptly.
- Screening for Co-occurring Disorders: Individuals undergoing detox should be screened for co-occurring mental health disorders, as these can complicate the detox process. Integrated treatment for both substance use and mental health issues may be necessary.
- Post-Detoxification Care: Transitioning from detox to ongoing treatment is critical for long-term recovery. A comprehensive aftercare plan should be in place, including counseling, therapy, and support groups.
These precautions help ensure the safety and effectiveness of medically assisted detoxification, supporting adults in their journey toward recovery from substance use disorders.
Available Treatments for Opioid Addiction
Opioid withdrawal is a challenging and often painful experience that individuals with opioid dependence face when trying to break free from the cycle of addiction. Fortunately, various effective treatment options are available to help manage and alleviate medical conditions.
Outpatient vs. Inpatient Treatment
One of the first decisions individuals must make when seeking treatment for opioid withdrawal is whether to opt for outpatient or inpatient treatment. Outpatient treatment allows individuals to receive care while continuing to live at home, providing flexibility and minimizing disruptions to daily life.
This option is suitable for those with a strong support system and a milder form of opioid dependence. On the other hand, inpatient treatment involves staying at a rehabilitation facility providing round-the-clock care and support.
This is often recommended for individuals with severe opioid dependence, co-occurring mental health issues, or those lacking a stable home environment. The choice between outpatient and inpatient settings depends on the individual’s specific needs and the severity of their withdrawal symptoms.
Therapy and Counseling
According to research and recent studies, therapy and counseling play a crucial role in the treatment of substance abuse by addressing the psychological aspects of addiction or mental illness.
Behavioral therapies such as cognitive-behavioral therapy (CBT) and contingency management help individuals identify and change negative patterns of thinking and behavior associated with drug use.
Group therapy provides a supportive environment where individuals can share their experiences, learn from others, and build community. Individual counseling allows for personalized treatment plans, addressing specific issues and triggers that contribute to opioid use disorder.
Combining these therapeutic approaches helps individuals develop coping strategies, manage stress, and build a foundation for long-term recovery.
Frequently Asked Questions (FAQ)
What is one medication used to treat opioid dependence?
Buprenorphine, an FDA-approved medication, is commonly used to treat opioid overdose and addiction. It alleviates withdrawal symptoms and cravings, helping individuals in recovery. Often administered as a sublingual film or tablet, it acts as a partial opioid agonist, reducing the risk of misuse.
Combining buprenorphine with counseling and support enhances its effectiveness in managing acute opioid withdrawal.
Do stimulants help ease the effects of opiate Withdrawal?
Stimulants may temporarily alleviate some opiate withdrawal symptoms, such as fatigue and lethargy, by increasing alertness and energy levels. However, they do not address the root cause of opiates and can exacerbate certain side effects. Comprehensive treatment, including medical supervision and support, is essential for managing opiate withdrawal symptoms effectively.
How do you prevent withdrawal symptoms?
To prevent withdrawal symptoms, gradually taper off substances under medical supervision. Stay hydrated, maintain a balanced diet, and engage in regular exercise. Seek medical treatment and support from friends, family, or a support group.
Consult healthcare professionals for personalized guidance. Follow a consistent sleep schedule, practice stress-reduction techniques, and consider therapy. Always prioritize your well-being and consult a healthcare professional for advice tailored to your situation.
Celebrate Opioid-Free life with The Haven Detox-Little Rock
Step onto a path to liberation with The Haven Detox-Little Rock, where resilience meets recovery.
Our expert therapists provide personalized care and support every step of the way. Our detox program ensures a safe and comfortable withdrawal process, while our residential treatment offers a structured environment for long-term recovery.Call us at (501) 271-3342 today, and let healing begin.





